Nephrology Doctor In Hyderabad
Nephrology (from Greek nephros meaning "kidney", logy meaning "the study of") is a specialty of medicine that concerns itself with the study of normal kidney function, kidney problems, the treatment of kidney problems and renal replacement therapy (dialysis and kidney transplantation). Disease conditions that affect the kidneys (such as diabetes, autoimmune diseases) and systemic problems that occur as a result of kidney problems (such as renal osteodystrophy and hypertension) are also studied in nephrology. A physician who has undertaken additional training to become an expert in nephrology is called a Nephrologist or a Renal physician. The term "nephrology" was first used in 1954.
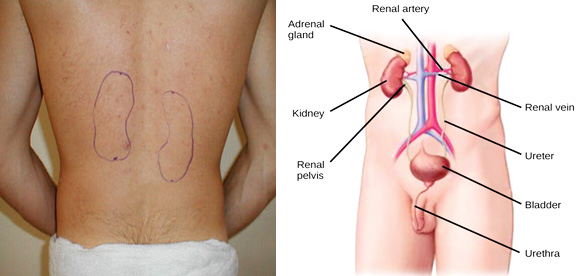
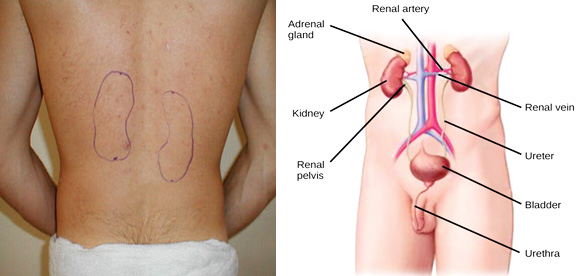
The kidneys’ function is to cleanse the blood of toxins. The kidneys ‘weigh only about 1% of our body weight. Yet, they receive 20% of the blood supply. The kidneys remove wastes, control the body's fluid balance, keep the bones healthy, initiate the production of red blood cells, and regulate the balance of electrolytes. As the kidneys filter blood, they create urine, which drains down tubes called ureters to the bladder.
Each kidney contains around a million units called nephrons, each of which is a tiny filter for blood. It's possible to lose as much as 90% of kidney function without experiencing any symptoms or problems. The kidneys produce a filtrate of about 180 litres per day, of which about 2 to 3 litres are passed out as urine.
The kidneys main functions are
- Excretory: removing the toxic wastes from the body into urine
- Hemodynamic: keeping the blood pressure under control
- Homeostatic: keeping the house (body) orderly. Managing sodium, calcium, acids etc
- Endocrine: producing hormones like erythropoietin, vitamin D etc
- Water balance: excreting excess water or withholding water when dehydrated
The kidneys are bean shaped structures of about 10 – 12 cm in length. They are situated at the back of the abdominal cavity, on either side of the spine. The left kidney is situated approximately at the vertebral level T12 to L3, and the right is slightly lower.
What is Chronic Kidney Disease?
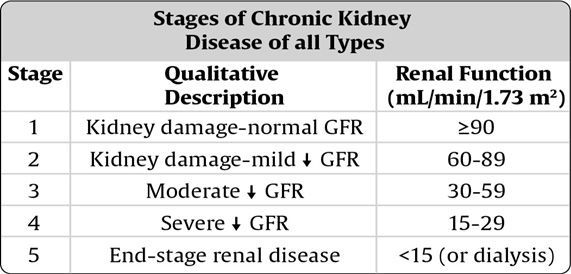
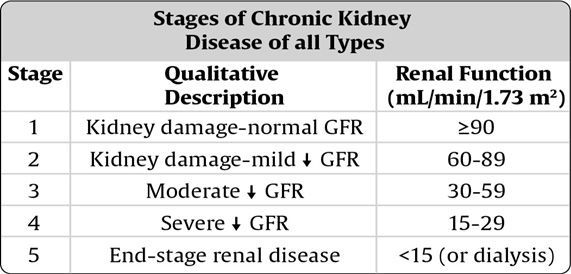
Slow, progressive and irreversible damage to the kidneys due to any cause resulting in gradual decrease in kidney function is called Chronic Kidney Disease (CKD). If kidney disease gets worse, wastes can build up to high levels in our blood. We may develop complications like high blood pressure, anemia (low hemoglobin), weak bones, poor nutritional health and nerve damage. Chronic kidney disease also increases the risk of having heart attacks and brain strokes. These problems may happen slowly over a period of time. Early detection and treatment can often keep chronic kidney disease from getting worse. As kidney disease progresses it eventually leads to kidney failure thus requiring dialysis or kidney transplantation.
The working of the kidneys is measured by a simple blood test called creatinine. In normal adults the serum creatinine is usually below 1mg/dl. This corresponds to 100% functioning of the kidneys. The functioning is usually talked about in terms of GFR (glomerular filtration rate). To know your kidney function, use the KIDNEY FUNCTION CALCULATOR. A normal adult male will have a kidney function of about 125 ml/min of GFR. A female of the same age and weight will have about 15% lesser i.e. 110 ml/min of GFR (due to lesser muscle mass). As kidney function or GFR decreases, the creatinine increases. Surprisingly, a creatinine of just 1.5 mg/dl corresponds to a GFR of about 60, a loss of 50% function!! A creatinine of 2 mg/dl is about GFR 30, creatinine of 3 mg/dl is about GFR 20, a creatinine of 4 mg/dl is about GFR 15 and a creatinine of 5 mg/dl is about GFR 10. If a patient’s GFR falls below 10, the excretion of toxic wastes is no longer adequate to maintain life and should be considering dialysis or kidney transplantation.
What are the Causes of Chronic Kidney Disease?
The common causes of CKD are
- Diabetes (up to 50% have diabetes as a cause of CKD)
- Hypertension
- Medications (like chronic pain killer usage, other kidney toxic medications)
- Nephrotic syndromes (loss of proteins in urine)
- Glomerulonephritis (loss of blood and proteins in urine)
- Hereditary conditions (like polycystic kidneys)
- Obstruction to kidneys (stones, cancers, strictures etc)
- Chronic kidney infections
- Unknown causes
What are the symptoms of Chronic Kidney Disease?
Most organs in our body, including the kidneys, do not cause any symptoms until more than 80 – 90% of the organ is damaged. Hence waiting for symptoms to check oneself maybe too late to detect treatable conditions. However the following symptoms may herald CKD
- Breathlessness upon walking short distances
- Breathlessness upon lying down
- Frothy or foamy urine
- Blood in urine
- Swollen feet and ankles
- Puffiness around eyes, especially in the morning
- Need to urinate more often, especially at night.
- Passing less urine especially less than 500 ml in a day
Anyone can get chronic kidney disease at any age. However, some people are more likely than others to develop kidney disease. You may have an increased risk for kidney disease if you:
- have diabetes
- have high blood pressure
- have a family history of kidney failure
- are older
- Taking pain killers often
- Diagnosed with chronic disease conditions like Rheumatoid arthritis, SLE
How is Chronic Kidney Disease detected?
Some simple tests can be done to detect early kidney disease. They are:
- A test for protein in the urine. Albumin to Creatinine Ratio (ACR), estimates the amount of albumin lost in your urine per day. An excess amount of protein in your urine may mean your kidney's filtering units have been damaged by disease. A positive result could be due to fever or heavy exercise, so your doctor will want to confirm your test over several weeks.
- A test for blood creatinine. The serum creatinine, along with age, race, gender and other factors, is used to calculate the Glomerular Filtration Rate (GFR). GFR calculator, click here.
How is Chronic Kidney Disease treated?
Strict control of diseases like diabetes, high blood pressure, cholesterol along with the required fluid intake, therapy for anemia, treatment for uric acid, therapy for acidosis can help to prevent kidney disease from getting worse. Kidney stones and urinary tract infections can usually be treated successfully. The exact causes of some kidney diseases are still unknown and specific treatments are not yet available for them. Treating high blood pressure with special medications called angiotensin converting enzyme (ACE) inhibitors or Angiotensin Receptor Blockers (ARBs) helps to slow the progression of chronic kidney disease. The Nephrologist will help to tailor your therapy as the case maybe. Sometimes, chronic kidney disease may progress to kidney failure, requiring dialysis or kidney transplantation.
How is Kidney Failure Treated?
Kidney failure may be treated with hemodialysis, peritoneal dialysis or kidney transplantation. Treatment with hemodialysis may be performed at a dialysis unit or at home. Hemodialysis treatments are usually performed three times a week. Peritoneal dialysis is generally done daily at home. Automated Peritoneal Dialysis (APD) requires the use of a machine while Continuous Ambulatory Peritoneal Dialysis (CAPD) does not. The Nephrologist will explain the different therapies and help individual patients make the best treatment choices for themselves and their families.
Kidney transplants have high success rates. The donor kidney could be from someone who is brain dead (termed Deceased Donor or Cadaver) or from a living donor, who may be a blood relative or unrelated.
Facts about Chronic Kidney Disease (CKD)
- One out of every 9 adults have CKD
- Early detection can help prevent the progression of kidney disease to kidney failure
- Heart disease is the major cause of death for all people with CKD
- Hypertension causes CKD and CKD causes hypertension.
- Persistent proteinuria (protein in the urine) means CKD is present
- High risk of kidney failure includes those with diabetes, hypertension and family history of kidney failure
- Two simple tests can detect CKD: Urine protein and serum Creatinine
- Glomerular filtration rate (GFR) is the best estimate of kidney function
Acute Kidney Injury
Acute kidney injury means the sudden loss of kidney function due to any cause. Acute kidney injury occurs when the kidneys become suddenly unable to filter waste products from the blood. When the kidneys lose their filtering ability, poisonous wastes accumulate in the blood.
Acute kidney injury — also called acute renal failure — can develop rapidly over a few hours to a few days. Acute kidney injury is most common in people who have been hospitalized, particularly into intensive care.
Acute kidney injury can be fatal and requires intensive treatment. However, acute kidney injury is usually reversible. Most people recover normal or nearly normal kidney function.
Signs and symptoms
- Decreased urine output, though sometimes urine output maybe normal
- Fluid retention, causing swelling of feet and body
- Breathlessness
- Drowsiness
- Fatigue
- Confusion
- Seizures or coma
Sometimes acute kidney injury causes no signs or symptoms and is detected through lab tests done for another reason.
Causes
Acute kidney injury can occur due to
- Decreased blood flow to the kidneys (pre-renal)
- Direct damage to the kidneys (renal)
- Blockage of urine from the kidneys (post-renal)
Decreased blood flow to the kidneys
- Blood loss from major bleeding
- Dehydration (sunstroke, diarrhea)
- Blood pressure medications (ACE inhibitors etc)
- Infection
- Liver injury
- Allergy to drugs
Direct damage to the kidneys
- Blood clots in the veins and arteries of the kidneys
- Cholesterol deposits that block blood flow in the kidneys
- Glomerulonephritis
- Vasculitis, an inflammation of small blood vessels
- Infection
- Medications like chemotherapy drugs, antibiotics, radiocontrast agents
- Multiple myeloma, a cancer of the plasma cells
- Toxins like heavy metals
Blockage of urine from the kidneys (urinary obstruction)
- Kidney stones
- Cancers of bladder, prostate, cervix, colon
- Nerve damage involving the nerves that control the bladder
Risk factors
- Hospitalization, especially for serious conditions requiring intensive care
- Advanced age (low GFR to start with)
- Vascular disease
- Diabetes
- Hypertension
- Heart injury
- Pre existing kidney disease
- Liver disease
Complications
- Fluid overload: Buildup of fluid in the lungs, which can cause shortness of breath.
- Electrolyte abnormalities: Derangements of potassium, sodium, calcium, magnesium, pH, acid balance, lactic acid are usually seen
- Permanent kidney damage: Rarely, AKI can cause permanent kidney loss of function, or end-stage renal disease. People with end-stage renal disease require either life-long dialysis or a kidney transplant to survive
- Death: Acute kidney injury can lead to loss of kidney function and, ultimately, death. The risk of death is higher in people who had kidney problems before acute kidney injury.
Tests
- Urine tests: Analyzing a sample of the urine, may reveal abnormalities that suggest the cause of kidney injury
- Blood tests: A sample of the blood may reveal rapidly rising levels of urea and creatinine — two substances used to measure kidney function. Other blood tests maybe done to look for electrolyte abnormalities, acidosis, sepsis, antibodies etc
- Imaging tests: Imaging tests such as ultrasound and computerized tomography may be used to help the doctor to assess the extent of damage to the kidneys
- Removing a sample of kidney tissue for testing: In some situations, the doctor may recommend a kidney biopsy to remove a small sample of kidney tissue for lab testing.
Treatment
Treatment for acute kidney injury typically requires a hospital stay. Most people with acute kidney injury are already hospitalized. The length of hospital stay depends on the causes for the acute kidney injury and how quickly the kidneys recover.
Treating the underlying cause of the kidney injury
Treatment for acute kidney injury involves identifying the illness or injury that originally damaged the kidneys. The treatment options depend on what's causing the kidney injury.
Treating complications until the kidneys recover
The doctor will also work to prevent complications and allow the kidneys time to heal. Treatments that help prevent complications include:
Treatments to balance the amount of fluids in the blood. If the acute kidney injury is caused by a lack of fluids in the blood, the doctor may recommend intravenous (IV) fluids. In other cases, acute kidney injury may result in too much fluid accumulation, leading to swelling in the arms and legs. In these cases, the doctor may recommend medications (diuretics) to expel excess water.
Medications to control blood potassium. If the kidneys aren't properly filtering potassium from the blood, the doctor may prescribe potassium binders to prevent the accumulation of high levels of potassium in the blood. Too much potassium in the blood can cause dangerous irregular heartbeats (arrhythmias) and even death.
Medications to restore blood calcium levels. If the levels of calcium in the blood drop too low, the doctor may recommend an infusion of calcium.
Dialysis: If toxins build up in the blood, temporary hemodialysis may be required to help remove toxins and excess fluids from the body while the kidneys heal. Dialysis may also help remove excess potassium from the body. During dialysis, a machine pumps blood out of the body through an artificial kidney (dialyzer) that filters out waste. The blood is then returned to the body.
Depending on the severity of the illness and other medical considerations, one out of several modalities of dialysis may be chosen. These are
- Hemodialysis (HD)
- Slow low efficiency hemodialysis (SLED)
- Peritoneal dialysis (PD)
- Extended daily diafiltration (EDDf)
- Continuous renal replacement therapy (CRRT)
What is diabetic nephropathy?
Progressive damage to the nephrons in the kidney due to diabetic damage, manifested by protein loss in urine and rising creatinine is Diabetic Nephropathy
Each human kidney is made of one million tiny filters called nephrons which filter blood, remove waste from the body and control fluid balance. In people with diabetes these nephrons slowly and progressively start to get damaged and begin to leak proteins (albumin) into the urine. This type of progressive kidney disease is called Diabetic nephropathy and most often results in kidney failure. Albumin in the urine is measured to diagnose and determine the progression of diabetic nephropathy. It is seen in both type 1 and type 2 diabetes. With early treatment, one can slow the progression of the disease. Once diabetic nephropathy sets in, kidney function can decrease at the rate of 10-15% per year. Most patients who have diabetic nephropathy will end up in kidney failure.
Disease progression depends on many factors. Some factors which increase the risk are
- Uncontrolled blood sugar
- Duration of the diabetes
- High blood pressure
- Family history of kidney disease
- Smoking
- Overweight
What are the symptoms of diabetic nephropathy?
Symptoms may not be noticed in the early stages of kidney damage. Some of the symptoms are
- Swelling of feet and ankles
- Breathlessness
- Fatigue most of the time
- General weakness
- Loss of appetite
- Itchy and dry skin
- Nausea or vomiting
What are the tests to diagnose diabetic nephropathy?
People with diabetes should undergo yearly health checkup to detect early signs of kidney damage as diabetes is one of the major causes for kidney failure. Common tests include:
- Urine examination: albumin or protein shown as ++ or 4+ etc
- Urine albumin – creatinine ratio
- Urine protein – creatinine ratio (when albumin is very high)
- Blood urea
- Serum creatinine
- Eye examination to look for retinopathy
- Kidney biopsy (if needed)
Treatment
Medications like ACE (Angiotensin-converting enzyme) inhibitors, angiotensin receptor blockers (ARBs) which decrease blood pressure as well as the pressure in the nephrons, are prescribed, thereby, protecting the nephrons from high pressure damage.
Other blood pressure medications may also be prescribed to keep the blood pressure under strict control. The damage to the kidneys worsens if blood pressure rises and conversely, blood pressure rises if kidney damage increases, setting off a vicious circle.
Other precautions that can help to slow down the progression are
- Regular monitoring of blood sugar levels (use a glucometer)
- Regular exercise (running, jogging, walking, swimming, badminton, cycling)
- Quit smoking
- Avoid pain-killers
- Weight loss (to a BMI of 24)
- Proper scientific diet
Nephrotic syndrome is a kidney disorder in which the kidneys excrete (leak) too much protein in urine.
Nephrotic syndrome is usually caused by damage to the small filters in the kidneys, called nephrons, which filter waste and excess water from the blood. Nephrotic syndrome causes swelling (edema) in the feet, face and sometimes the whole body.
Treatment for nephrotic syndrome includes treating the underlying condition that is causing it. Nephrotic syndrome can increase the risk of infections and blood clots. The condition may medications and dietary changes to prevent these and other complications of nephrotic syndrome.
Signs and symptoms of nephrotic syndrome include:
- Severe swelling (edema), particularly around the eyes and in the ankles and feet
- Foamy or frothy urine, which may be caused by excess protein in the urine
- Weight gain due to excess fluid retention
The nephrons filter the blood as it passes through the kidneys. Of the 180 liters of filtrate per day, the kidneys reabsorb up to 98% back, while excreting the remaining toxic wastes. Healthy nephrons hold back the protein (mainly albumin) — which is needed to maintain the right amount of fluid in the body — from seeping into the urine. When damaged, these nephrons leak high amounts protein into the urine, leading to nephrotic syndrome.
Many possible causes
Many diseases and conditions can cause damage to nephrons and lead to nephrotic syndrome, including:
- Minimal change disease. This is the most common cause of nephrotic syndrome in children, this disorder results in abnormal kidney function, but when the kidney tissue is examined under a microscope, it appears normal or nearly normal.
- Focal segmental glomerulosclerosis. Not a very benign condition, the filtering membrane of the nephrons becomes thick and lumpy and tends to lose protein. This condition can frequently lead to kidney failure if not treated adequately.
- Membranous nephropathy. This is the result of thickening of the membranes within the glomeruli. The exact cause of the thickening isn't known, but it's sometimes associated with other medical conditions, such as hepatitis B, malaria, lupus and cancer.
- Diabetic kidney disease. Diabetes can lead to kidney damage (diabetic nephropathy) that affects the glomeruli and commonly lead to kidney failure.
- Systemic lupus erythematosus. This auto-immune antibody mediated inflammatory disease can lead to serious kidney damage.
Factors that can increase the risk of nephrotic syndrome include:
- Medical conditions. Certain diseases and conditions increase the risk of developing nephrotic syndrome, such as diabetes, lupus, amyloidosis, minimal change disease and other kidney diseases.
- Certain medications. Examples of medications that can cause nephrotic syndrome include nonsteroidal anti-inflammatory drugs (pain killers) and some antibiotics.
- Certain infections. Examples of infections that increase the risk of nephrotic syndrome include HIV, hepatitis B, hepatitis C and malaria.
Complications
Possible complications of nephrotic syndrome include:
- Blood clots. The inability of the glomeruli to filter blood properly can lead to loss of blood proteins that help prevent clotting. This increases the risk of developing a blood clot (thrombus) in the veins.
- High blood cholesterol and elevated blood triglycerides. When the level of the protein albumin in the blood falls, the liver makes more albumin. At the same time, the liver releases more cholesterol and triglycerides.
- Poor nutrition. Loss of too much blood protein can result in malnutrition. This can lead to weight loss, but it may be masked by swelling. May also lead to anemia and low levels of vitamin D and calcium.
- High blood pressure. Damage to the glomeruli and the resulting buildup of wastes in the bloodstream (uremia) can raise the blood pressure.
- Acute kidney failure. If the kidneys lose their ability to filter blood due to damage to the glomeruli, waste products may build up quickly in the blood. If this happens, emergency dialysis maybe needed.
- Chronic kidney disease. Nephrotic syndrome may cause the kidneys to gradually lose their function over time. Kidney function falls low enough, requiring dialysis or a kidney transplant.
- Infections. People with nephrotic syndrome have an increased risk of infections.
Diagnostic tests
- Urine tests.
Complete urine examination will show protein or albumin as +++ or 4+ etc.
Urine (spot sample) protein creatinine ratio
24-hour collection of urine for proteinuria
- Blood tests.
Blood tests may show
Low levels of the protein
Low albumin (hypoalbuminemia)
Increase in blood cholesterol and blood triglycerides
Increased serum creatinine and blood urea
Deranged serum electrolytes (sodium, potassium, calcium, magnesium)
- Kidney biopsy. The doctor may recommend a procedure called a kidney biopsy to remove a small sample of kidney tissue for testing. During a kidney biopsy, a special needle is inserted through the skin and into the kidney. Kidney tissue is collected and sent to a lab for testing.
Treatment
Treatment for nephrotic syndrome involves treating any underlying medical condition that may be causing the nephrotic syndrome. The doctor may also recommend medications that may help control the signs and symptoms or treat complications of nephrotic syndrome. Medications may include:
- Blood pressure medications. Drugs called angiotensin-converting enzyme inhibitors reduce blood pressure and also reduce the amount of protein released in urine. Medications in this category include benazepril (Lotensin), captopril (Capoten) and enalapril (Vasotec). Another group of drugs that works in a similar way is called angiotensin II receptor blockers and includes losartan (Cozaar) and valsartan (Diovan).
- Diuretics. Water pills (diuretics) help control swelling by increasing the kidneys' fluid output. Diuretic medications include furosemide (Lasix) and spironolactone (Aldactone).
- Cholesterol medications. Medications called statins can help lower cholesterol levels. However, it's currently unclear whether or not cholesterol-lowering medications can specifically improve the outcomes of people with nephrotic syndrome, such as avoiding heart attacks or decreasing the risk of early death. Statins include atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Altoprev, Mevacor), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor).
- Blood thinners. Medications called anticoagulants help decrease the blood's ability to clot and reduce the risk of developing blood clots. Anticoagulants include heparin or warfarin (Coumadin).
- Immune system-suppressing medications. Medications to suppress the immune system, such as steroids, cyclosporine, tacrolimus, cyclophosphamide, mycophenolate etc may be used.
Diet
Recommend that:
- High protein diet (to offset the losses in urine)
- Reduce the amount of fat and cholesterol in the diet to help control the blood cholesterol levels
- Low-salt diet to help control the swelling (edema) and blood pressure
- Fluid restriction depending on the amount of swelling